Engineering inventions to improve health date back at least to 1850, when the famous physicist Hermann von Helmholtz devised the ophthalmoscope. One of the first medical devices, it allows a doctor to look at the interior of a patient’s eye. In the latter part of the 20th century the pace of innovation in medical devices increased dramatically, with a global market size estimated at $321 billion in 2012.
Here are three heroic pieces of medical device technology which save or improve countless lives every day: the pacemaker, the insulin pump, and the defibrillator.
The Pacemaker
A normal, healthy heart controls the rate and rhythm of the heartbeat with its internal electrical system. Signals travel from the top to the bottom of the heart creating effective movement of blood. When this mechanism goes wrong, the signaling must be supplemented or replaced. This was the impetus behind the invention of the pacemaker (Figure 1). It senses when the heartbeat deviates from a healthy rhythm and generates corrective electrical pulses in the heart muscle.
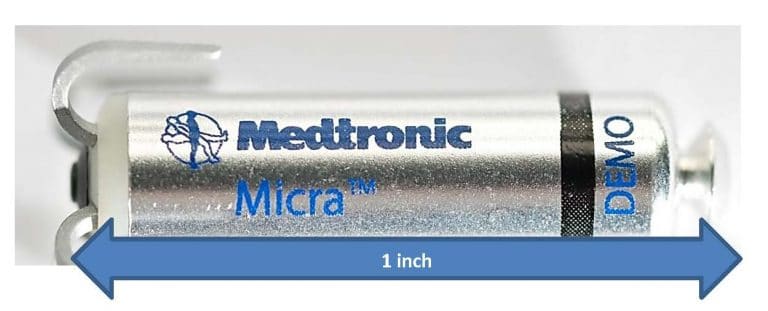
Today’s pacemakers are remarkable for their tiny size and long life. They can be implanted without major surgery and no longer require leads, which increases reliability. Pacemakers are also highly programmable, allowing their operation to be tailored to the needs of each patient. The increase in length and quality of life produced by these devices is profound.
Insulin Pumps
Insulin is a vital hormone which regulates the sugar in the blood, which is critical to health. But 220 million people in the world suffer from diabetes, and must supplement their insulin deficiency. Most often this is done through injections, which cause swings in the blood’s glucose level. Large variations can cause serious medical complications and even death, so what is needed is a way to provide the patient with a steady infusion of the hormone. The pump of Figure 2 does this important job.
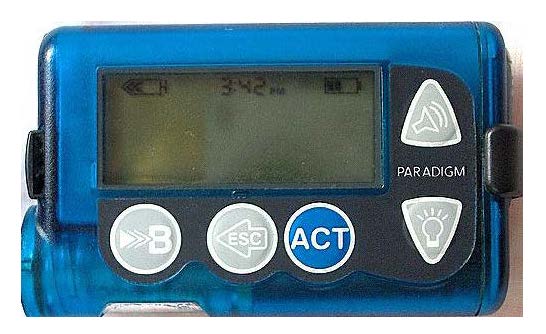
Such pumps automate blood sugar management by delivering a measured, continuous dose, or a burst needed at mealtimes. Insulin is delivered through a flexible plastic tube inserted through the skin. With this device, patients need not give themselves individual insulin injections. Since it reduces blood glucose variation throughout the day, it is a big advance in safety. And it improves the patient’s quality of life.
Heart Defibrillator
Sudden cardiac arrest—when the heart fails to contract effectively—results in loss of consciousness and breathing and death within a few minutes. Each minute before treatment starts cuts the chances of survival by 10%.
Automated external defibrillators (AEDs) sense whether the heart is beating in an ineffective way and deliver a shock which jolts the heart, prompting it to pump again. They are called defibrillators because they combat the dangerous heart condition known as ventricular fibrillation. The urgent need is to get the heart out of fibrillation and back to pumping blood.
These devices are designed to be used by untrained bystanders. They have audio instructions and safety circuits to ensure that shocks are not produced if medically inappropriate (Figure 3).

The basic technology for heart defibrillation was discovered way back in 1899 by two Swiss physiologists. Later improvements by biomedical engineers allowed the paddles to be placed on the chest, without direct contact with the heart. More recent innovations—detecting what, if anything is wrong with the patient’s heart—greatly reduced the skills needed to successfully operate the defibrillator.
Litigation in medical devices which may require a medical device expert witness
Medical devices have obvious, often life-saving benefits. Sadly, when things go wrong, bad things can happen. This causes substantial medical device litigation, which often turns on highly technical matters. In these cases lawyers frequently turn to expert witnesses for assistance. Here are some examples:
Duodenoscopes are an optical device fed down patients’ throats to treat or diagnose various gastrointestinal ailments. Unfortunately, bacteria can harbor in small crevasses in a duodenoscope and may not be removed even after manufacturer-recommended cleaning and disinfecting is performed. This has allegedly caused dozens of infections and deaths.
A study of the safety of surgical robots has linked the machines’ use to at least 144 deaths and over 1,000 injuries over a 14-year period in the USA.
Inferior Vena Cava filters catch blood clots before they move into the lungs. Roughly 200,000 blood clot filters are implanted to prevent pulmonary embolisms each year, but the complication rate may be higher than previously recognized. Many lawsuits have been filed against their manufacturers, alleging punctured veins and organs, fractured devices, and chronic health issues.
In addition to product liability claims, technology used in medical devices may become subject to patent litigation. In such cases a medical device patent expert witness is commonly employed to testify on issues such as validity and infringement.
References
Duodenoscope: Newton v. Olympus America, Inc., Court of Common Pleas, Philadelphia County, PA, Mar 19, 2015. Case ID 150302493.
Robotic surgery: H. Alemzadeh et al., “Adverse Events in Robotic Surgery: A Retrospective Study of 14 Years of FDA Data.” Presented at the 50th Annual Meeting of the Society of Thoracic Surgeons, January 2013. Article available online.
Inferior Vena Cava filters: In Re: Bard IVC Filters Products Liability Litigation, 2:15-md-02641, October 30, 2015, United States District Court for the District of Arizona.
Leave a Reply